Dental implants may sometimes fail due to reasons like gum infection around the implant (peri-implantitis), incomplete bone integration, or improper chewing forces. Other factors contributing to dental implant failure include smoking, uncontrolled diabetes, or insufficient dental expertise. Warning signs, such as implant looseness, persistent pain, swelling, or bleeding around the implant, require immediate dental attention.
Maintaining excellent oral hygiene with implant-specific brushes and floss is crucial. Regular 6-month check-ups and professional cleanings significantly boost implant longevity. Smokers should consider quitting to improve success rates. Most importantly, choosing an experienced implant specialist significantly reduces the potential for complications.
In this blog post, we’ll explore failed implant treatment —how to recognize it, what causes it, and how to ensure you receive the best possible treatment for your oral health.
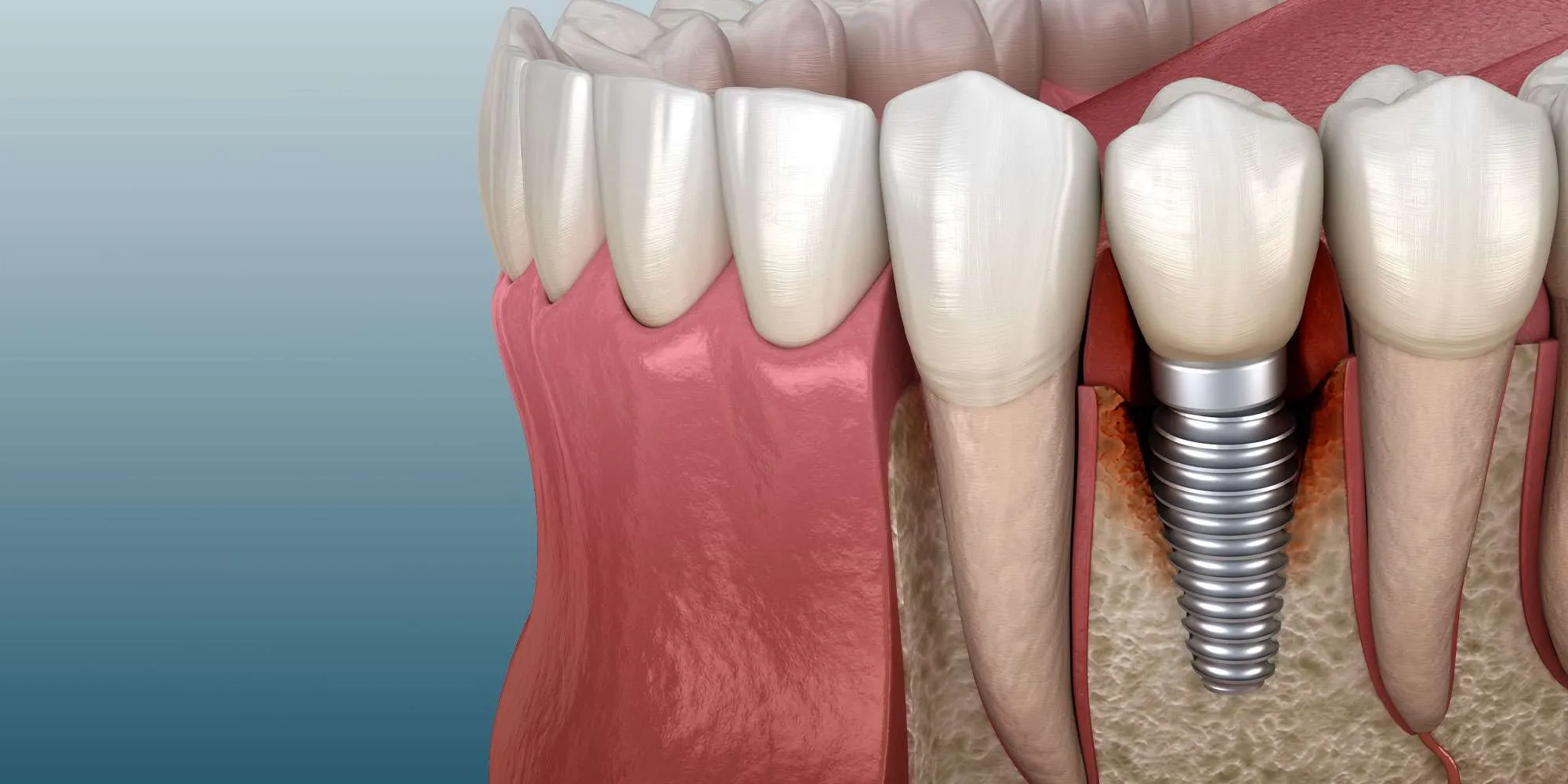
Common Causes of Implant Failure
Dental implants can fail for several key reasons. The most common cause is gum infection around the implant (peri-implantitis), which occurs due to bacterial buildup and poor oral hygiene. Other factors leading to dental implant failure include failed bone integration, improper chewing forces, and medical conditions like uncontrolled diabetes or osteoporosis. Technical errors during surgery, such as incorrect implant placement or damage to surrounding tissues, may also cause treatment failure.
To keep your dental implant healthy and complication-free for decades, follow these key guidelines: 1) Use implant-specific brushes and floss daily for optimal cleaning, 2) Never miss your twice-yearly professional check-ups and cleanings at our Watertown or Wayland office, and 3) Quit smoking and properly manage conditions like diabetes that can affect healing. Most importantly, choose an experienced implant specialist – at D’Amico Dental Care, our expertise helps ensure your implant enjoys a long, trouble-free lifespan while maintaining your beautiful smile.
Signs of Dental Implant Failure
If you notice any signs of implant failure, such as these symptoms after getting a dental implant, they might indicate trouble. Contact your dentist immediately if you observe – early intervention can prevent complications. Your dentist may prescribe antibiotics or, in severe cases, remove the implant. Maintaining good oral hygiene and regular check-ups remains the best prevention strategy.
Early Warning Signs (1-4 weeks post-op):
✓ Severe persistent pain: Lasting beyond 5 days
✓ Abnormal swelling: Increasing after day 3
✓ Prolonged bleeding: Continuing past 48 hours
✓ Persistent numbness: Lasting over 2 weeks (indicating nerve damage)
Late Signs (after osseointegration):
✓ Loose implant: Detectable during clinical exam
✓ Bone loss: Visible on serial radiographs
✓ Peri-implantitis: Gum inflammation with bleeding/pus
✓ Mechanical dental implant failure: Fractured implant components
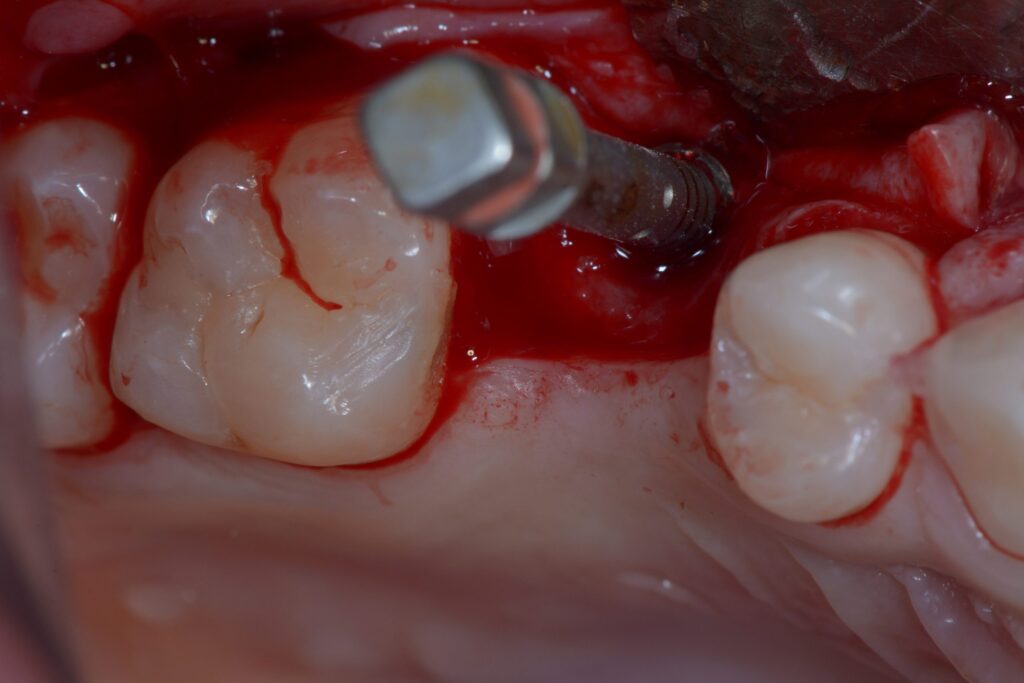
Severe Persistent Pain After Implant Surgery
Pain lasting more than 5 days after dental implant surgery is a major warning sign. While mild to moderate discomfort is normal for the first 3-4 days, intense throbbing pain unrelieved by standard medications may indicate infection, nerve damage, or severe inflammation. This pain often accompanies other symptoms like fever, increasing swelling, or pus discharge, requiring immediate dental evaluation. Importantly, implant-related infection pain typically worsens at night and may radiate to the ear or temple.
If experiencing such pain, see your dentist immediately, as it may indicate potential causes of implant failure, which they’ll diagnose through clinical examination and possibly X-rays. Treatment may involve antibiotics, infection drainage, or, in severe cases of dental implant failure, removal. Sometimes, persistent pain stems from improper implant pressure on bone or nerves, requiring adjustment or replacement. Preventing implant failure includes choosing an experienced surgeon, strict post-op care, and avoiding smoking/alcohol.
Abnormal Swelling After Implant Surgery
In cases of failed implant treatment, while some swelling is normal for the first 2-3 days post-surgery, swelling that intensifies or spreads after day three often indicates infection or severe inflammatory complications requiring immediate professional evaluation. This abnormal swelling typically comes with skin redness, warmth in the area, and throbbing pain. In acute cases, patients might experience mild fever. Swelling that worsens daily, especially when accompanied by difficulty opening the mouth, requires immediate attention.
This progressive swelling often results from bacterial infection, foreign body reaction, or abscess formation. Your dentist may prescribe antibiotics or, if an abscess forms, drain it. While cold compresses help initially (first 48 hours) and warm compresses afterward can reduce swelling, persistent swelling beyond 5 days demands professional evaluation. When left untreated, such swelling could contribute to dental implant failure. Prevention includes maintaining oral hygiene, taking prescribed antibiotics, and avoiding strenuous post-surgery activities.
Prolonged Bleeding After Implant Surgery
Some bleeding is normal for the first 24-48 hours after implant surgery, but bleeding beyond this period raises concerns as potential signs of implant failure that require professional evaluation. This could indicate blood clotting disorders, high blood pressure, surgical blood vessel damage, or developing infection. Continuous bleeding, unstopped by sterile gauze – especially with a metallic taste or large blood clots – requires immediate attention, as it might signal potential dental implant failure.
For ongoing bleeding:
- Apply moist sterile gauze with gentle pressure for 30 minutes
- Avoid spitting or vigorous rinsing
- Seek dental care if bleeding continues after 2 hours
Your dentist may use:
- Hemostatic agents
• Additional sutures
• Clotting medications (in rare cases)
Preventive measures:
✓ Patients with clotting disorders need pre-surgical evaluation
✓ Avoid blood thinners like aspirin before surgery
Persistent Numbness After Implant
Numbness that continues for more than two weeks after implant surgery often signals nerve damage, particularly in the lower jaw where the inferior alveolar nerve runs close to the roots. Patients typically describe this as a constant tingling (“pins and needles”) or complete loss of sensation in the chin or lower lip. This complication usually occurs when the implant puts pressure on the nerve, though swelling or (rarely) partial nerve tears can also be responsible. If left unaddressed, this condition could potentially lead to dental implant failure, making early intervention crucial.
Your dentist will evaluate the nerve damage through sensory tests and 3D scans (CBCT). Treatment options for failed implant treatment range from anti-inflammatory steroids and nerve-supporting vitamin B supplements to corrective surgery in severe cases. While full recovery may take 3-6 months, some nerve damage can be permanent. The best prevention involves careful pre-surgical planning using 3D imaging and maintaining at least 2mm of space between the implant and nerve canals to avoid compression.
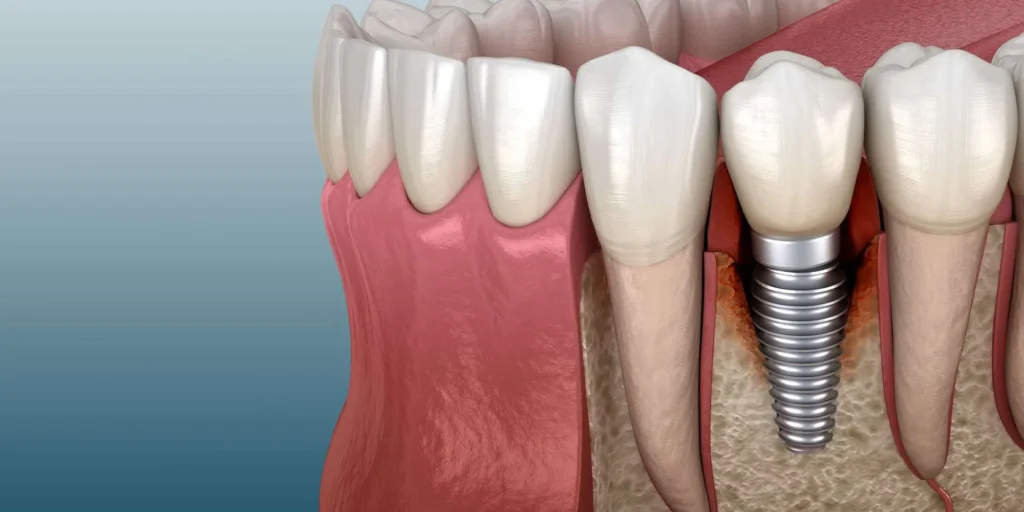
Loose Implant
When an implant moves during clinical examination, it’s one of the clearest signs of treatment problems. This typically occurs due to failed bone integration (osseointegration failure) or progressive bone loss around the implant. Dentists assess mobility using specialized tools like periodontal probes or controlled pressure tests. A loose implant often accompanies other symptoms like pain, gum inflammation, or visible position changes, which could ultimately lead to dental implant failure if unaddressed.
While implant failure can occur due to infection (peri-implantitis), premature loading, insufficient bone density, or surgical factors, our team at D’Amico Dental Care minimizes risks through precise CBCT-guided placement, customized healing protocols, and thorough patient education. Mild cases may be resolved with antibiotics and bite adjustments, but advanced failures often require implant removal, bone grafting, and delayed re-implantation. The key to long-term success lies in meticulous oral hygiene with implant-specific tools, strict adherence to post-op instructions, and regular professional cleanings at our Watertown or Wayland offices – following these guidelines helps ensure your implant remains healthy and functional for decades.
Bone Loss Around Implants
Progressive bone loss visible in consecutive X-rays serves as a critical warning sign for implant complications. While 0.5-1mm of annual bone loss is normal during the first year post-placement, excessive loss exceeding 2mm/year or visibly progressing in serial images indicates trouble. Radiographs typically reveal this as reduced bone density near the implant’s neck and dark spaces around it, which, if left unchecked, could ultimately lead to dental implant failure.
Multiple factors contribute to bone loss, including infection (peri-implantitis), excessive loading forces, improper prosthesis design, or adverse biological reactions to the implant. Without timely intervention, this deterioration may progress, causing implant loosening and complete failure. Preventing implant failure requires treatment involving infection control, bite force adjustments, and, preventing implant failure in advanced cases, implant removal with bone grafting, while regular radiographic monitoring every 6-12 months remains essential for early detection.
Peri-implantitis: A Serious Threat to Dental Implants
Peri-implantitis is a progressive inflammatory infection in the tissues surrounding an implant and one of the primary causes of implant failure, characterized by distinct symptoms that typically include gum inflammation, redness, bleeding during probing, and, in advanced cases, pus discharge from the area. A probing depth exceeding 4mm with bleeding, combined with visible bone loss on X-rays, confirms the diagnosis. If left untreated, this condition can lead to severe bone deterioration and ultimately dental implant failure, resulting in implant loss.
Treatment depends on the disease stage and may involve non-surgical approaches like scaling the implant surface with titanium tools, using local or systemic antibiotics, or surgical methods such as bone regeneration. Prevention is key—meticulous oral hygiene, specialized implant brushes and floss, and regular six-month check-ups can significantly reduce risks. Smokers and individuals with uncontrolled diabetes face a higher susceptibility to this complication.
Mechanical Failure of Dental Implants
Mechanical failure in dental implants typically appears as a fracture in one of the implant system’s components (fixture, abutment, or connecting screw), which can be signs of implant failure, often resulting from excessive forces due to teeth grinding (bruxism), improper prosthesis design, or material fatigue after years of use. The most severe type—fixture fracture—usually requires complete implant removal and bone grafting. Symptoms include sudden pain, a loose crown, and changes in bite alignment, all of which could contribute to dental implant failure if ignored.
Treatment depends on the fracture location: a broken screw can often be replaced, while abutment fractures may require full replacement. Prevention strategies include:
- Night guards for bruxism patients
- Proper prosthesis design to evenly distribute forces
- High-quality implants with appropriate diameters
Annual check-ups are vital for assessing component integrity and detecting microscopic cracks early.
Risk Factors for Implant Failure
Dental implant failure can stem from various factors, generally categorized into 4 groups – each potentially affecting your oral health and implant success:
- Systemic Factors: Uncontrolled diabetes (HbA1c>7), severe osteoporosis, blood clotting disorders, autoimmune diseases, jaw radiation therapy.
- Behavioral Factors: Smoking (triples risk), poor oral hygiene, teeth grinding (bruxism), and alcohol consumption.
- Local Factors: Insufficient bone density, active oral infections, poor gum quality, improper implant positioning.
- Technical Factors: Surgeon inexperience, poor prosthesis design, premature loading, incorrect implant size selection.
“ Pairwise meta-analysis showed that implants in smokers had a higher failure risk in comparison with non-smokers (OR 2.402, p < 0.001). The difference in implant failure between the groups was statistically significant in the maxilla (OR 2.910, p < 0.001), as well as in the mandible (OR 2.866, p < 0.001). “
How to Prevent Implant Failure?
To avoid dental implant failure, start with a comprehensive evaluation including oral exams, 3D imaging, and blood tests. Preventing implant failure involves controlling conditions like diabetes and quitting smoking at least one month before surgery, while precision techniques and advanced equipment such as digital surgical guides and bone temperature control are vital during the procedure. Post-surgery, strictly follow your dentist’s instructions: take prescribed antibiotics, use special mouthwash, and avoid putting pressure on the implant during initial healing.
For lasting results:
✓ Get professional cleanings and check-ups every 6 months
✓ Use a night guard if you grind your teeth
✓ Maintain excellent hygiene with proper brushing and implant-specific flossing
Following these guidelines boosts success rates to 98%, letting you enjoy your implant for decades without issues.
When to Seek Help: Consulting Your Dentist
If you experience severe pain that doesn’t improve with regular painkillers, or if swelling/redness worsens after 3 days, see your dentist immediately at D’Amico Dental Care. Other danger signs include:
- Bleeding lasting hours
- Prolonged facial numbness
- Fever/chills
Even minor issues like implant looseness or bad breath shouldn’t be ignored, as they might indicate early dental implant failure.
After your implant procedure, promptly contact our office if you experience red/swollen gums around the implant, chewing discomfort, pus discharge, noticeable implant movement, or temperature sensitivity – these may indicate complications needing attention. While regular 6-month check-ups at our Watertown or Wayland locations help prevent most issues, seek immediate emergency care for severe symptoms like facial swelling or breathing difficulties, as these require urgent treatment to protect both your implant and overall health.
FAQ
- What Factors Cause Dental Implant Failure?
- Bacterial infection (peri-implantitis): 45% of cases
- Failed osseointegration: 30% of cases
- Overloading: 15% of cases
- Surgical errors: 8% of cases
- Body rejection: 2% of cases
- How Can I Tell If My Implant Is Failing?
- Persistent pain beyond 1 week
- Noticeable implant mobility
- Swelling/inflammation around the implant
- Pus discharge from the implant site
- Visible bone loss on radiographs
- Which Controllable Behaviors Increase Failure Risk?
- Smoking (3x higher risk)
- Poor oral hygiene
- Non-compliance with post-op instructions
- Chewing hard foods during healing
- Skipping follow-up appointments
- What Medical Conditions Affect Implant Success?
- Uncontrolled diabetes (high blood sugar)
- Severe osteoporosis
- Blood clotting disorders
- Autoimmune diseases
- History of jaw radiation therapy
- What Are the Treatment Options for Failed Implants?
- Infection control with antibiotics and scaling
- Bone grafting and reimplantation after 3-6 months
- Wider diameter implant placement
- Sinus lift (for upper jaw implants)
- Alternatives like bridges or dentures
- How Can I Prevent Implant Failure?
- Choose an experienced specialist with proven success
- Quit smoking ≥2 weeks pre/post-surgery
- Meticulous oral hygiene maintenance
- Control systemic diseases like diabetes
- Avoid pressure on the implant during the initial months
- What Are Implant Success Rates?
- Overall: 95-98% at 5 years
- Lower jaw: 97% success
- Upper jaw: 94% success
- Smokers: 10-15% lower success
- With bone grafts: 85-90% success
- What Are the Replacement Costs If an Implant Fails?
- Manufacturer warranty: Typically 5-10 years (parts only)
- Clinic warranty: Varies by center
- Replacement cost: 30-50% of the original fee
- Insurance coverage: Usually limited/none
- Additional costs: Bone grafts, antibiotics